

13However, this was not the case when the drug was used at half the dose. h −1reduced postoperative morphine needs and the incidence of residual pain until the sixth postoperative month.
#Managing emergent phenomena with ketamine trial
In a long-term outcome trial on adenocarcinoma surgery with general or epidural anesthesia, racemic ketamine injected as a 0.5 mg/kg preincisional bolus followed by an infusion of 0.25 mg 1).ĭosing of ketamine when used for this purpose is affected by variety of factors, including the expected amount of pain, whether general or epidural anesthesia will be used, and whether ketamine will be applied intraoperatively or intraoperatively and postoperatively (level II evidence) ( table 1). Thus, the adequacy of the ketamine administration schedule is a crucial component for pain prevention ( fig. 18To prevent pathologic pain, ketamine needs to be applied at least throughout the operation and likely for a period of time into the postoperative phase, in an attempt to reduce sensitization of central and peripheral pain pathways. A single injection of a short-acting drug such as ketamine either before or after incision will therefore not provide analgesia that lasts far into the postoperative period.
However, nociceptive and inflammatory signals are generated throughout surgery and after the procedure. Studies have compared the effects of ketamine administration before surgery with those of one ketamine administration at the end of surgery to test its “preemptive” analgesic properties. 17Second, the dosing schedule may be inadequate. First, beneficial effects of ketamine may be masked when the drug is used in small doses (<0.15 mg/kg) against the background of multimodal or epidural analgesia.
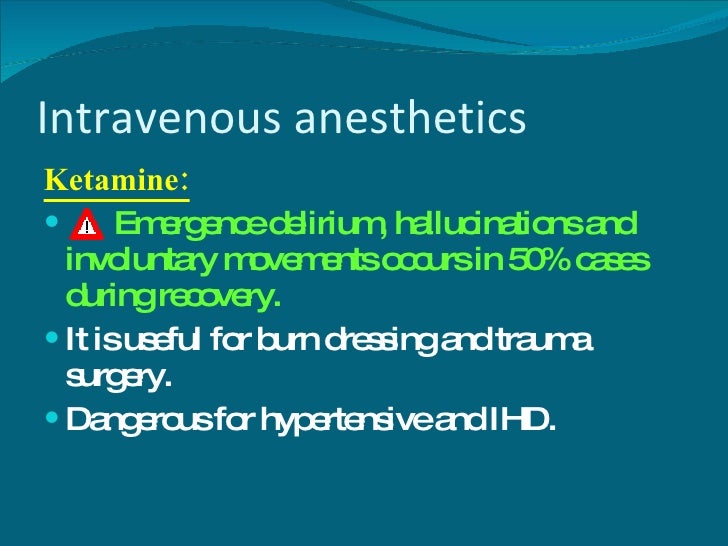
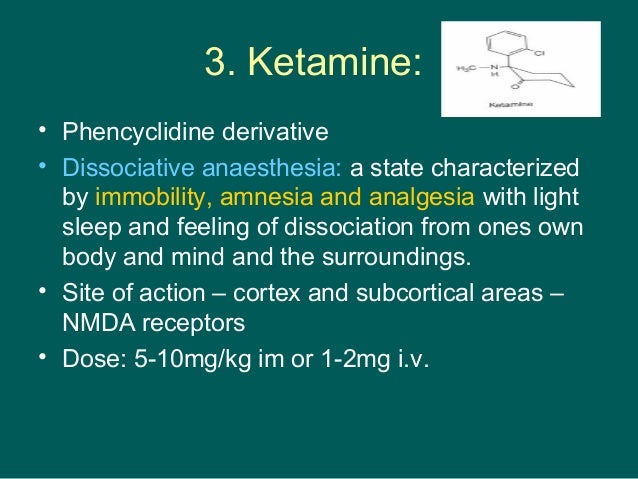
17,18Two factors may explain these failures. 9–16However, some studies did not show this benefit (level II evidence) ( table 1). Intravenous subanesthetic ketamine, when added as an adjunct to general anesthesia, reduced postoperative pain and opioid requirements in a variety of settings, from outpatient surgery to major abdominal procedures (level II evidence) ( table 1). 7Ketamine therefore represents a promising modality in several perioperative strategies to prevent pathologic pain. 5When studied at subanesthetic doses, its analgesic efficacy correlates well with its inhibiting action on NMDA receptor-mediated pain facilitation 4,6and a decrease in activity of brain structures that respond to noxious stimuli. 1–3Ketamine binds noncompetitively to the phencyclidine binding site of NMDA receptors 4but also modifies them via allosteric mechanisms. 1–3NMDA receptors participate in the development and maintenance of what can be called “pathologic pain” after tissue injury: increased pain perception as a result of pain sensitization, in part from synaptic plasticity. In particular, the role of N -methyl-d-aspartate (NMDA) excitatory glutamate receptors in nociceptive transmission has been established in humans. AS part of the effort to develop mechanisms-based approaches to pain therapy, renewed interest has focused on the use of ketamine for treatment of acute and chronic pain.


 0 kommentar(er)
0 kommentar(er)
